Introduction
Scleredema Diabeticorum is an infrequent connective tissue disorder characterized by thickening, hardening, and painlessness of the affection of skin, was first described by Buschke in the year 1900.1 The term scleredema is a misnomer because neither sclerosis nor edema is found on microscopic examination. Sometimes, it just presents with erythema and pigmentation of the skin without any clear demarcation between involved and normal skin.
There are three clinical forms of scleredema, which are classified by their associated condition are, associated with a history of an antecedent infection (type 1), a blood dyscrasia (type 2), or diabetes mellitus (type 3). Each of these clinical forms has a different history, course, and prognosis.2 Here we are reporting a care of scleredema with multiorgan involvement.
Case Report
This 44 years old female, obese, known case of type2 Diabetes mellitus usually well controlled with medication, was in apparently alright with good effort tolerance till 3 months back, when is noticed swelling over both feet which were pitting in nature initially and gradually progressed till trunk and abdomen, since last few days rapid progression was observed along with complains of distension of abdomen with non-pitting edema. Feet and abdomen were rock hard in consistency. Hyperpigmentation of skin started in lower extremities more on anterior and medial aspect of thighs since last 3 months but last 7 days it was looking blacker and redder and progressed to abdomen. There were blisters and vesicles (as seen in Figure 1, Figure 2, Figure 3) hence she got admitted to our hospital for further treatment.
Patient was extensively investigated. Her blood biochemistry were, (ESR 18, SGOT- 29, SGPT- 25, S. Bilirubin- 1.8,S.Albumin -3.08, WBC-18000, Hb- 13.6, platelets- 366, BNP- 2600, Creatinine- 0.6.) suggestive of slightly low albumin levels with leukocytosis with raised BNP indicating fluid overload which was confirmed on The 2 D echo revealing Generalized LV hypokinesia, dilated chamber, dilated IVC with reduced LVEF – 25 %. USG abdomen revealed hepatomegaly with moderate ascites.
Serology for RA, ANA, Anti DNA, ASMA, ENA profile, anti-mitochondrial antibody as part of connective tissue disorder work up done but were negative. For non-pitting edema work up for thyroid was in form blood level T3, T4, TSH was done but turn out be normal. Serum Electrophoresis showed raised band in Beta globulin region with raised serum IgG -1657 level indicating possible gammopathy, Bone marrow biopsy was done which ruled out Multiple Myeloma and it showed a reactive marrow with plasma cells 4 %. Even CT scan abdomen was done but could not add more, except suggestive of large amount of ascites and mild hepatomegaly.
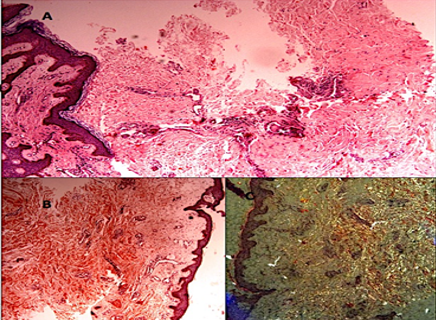
Hence finally skin biopsy was attempted after consulting dermatologist which was negative for Myeloma and Amyloid but findings were consistent with Scleredema as seen in Figure 4.
Management
After through and extensive investigation, Clinical and biopsy diagnosis of scleredema with LV dysfunction was made and patient started on Aldactone and Torsemide as well as ACE inhibitors. Patient was kept in negative balance more than 1000ml/day almost every day. In view of high WBC count and clinical picture patient was treated with Daptomycin to cover for a cellulitis and was deescalated and stop after 10 days. Patient was afebrile for 14 days during hospitalization. As patient was showing clinical improvement with passing good amount of urine without diuretics and was mobilized as walking with support as she was clinically stable. On 15day patient developed very high-grade fever of 105 F, without chills and rigors and became restless, progressively drowsy, breathless with decrease in urine output, was shifted to ICU for further management. In ICU X-ray chest showed bilateral basal haziness. Patient had severe hypotension required high doses of Noradrenaline, vasopressor supports. Patient became Anuric, K+ 6.9, ABG suggests severe acidosis, S. Bilirubin- 6.4, INR 6.4, Procalcitonin -3.5, SGOT- 17000, SGPT- 1800, WBC- 30000, suggestive of severe septic shock with multi-organ dysfunction. She was started with IV Meropenem and Vancomycin as broad-spectrum antibiotic cover and stress dose of steroid. Patient was electively intubated in view of hypoxia, acidosis and hemodynamic instability and put on ventilator. FFPs transfusions were given in view of very high INR. Patient was immediately dialyzed. ECG was initially sinus rhythm later showing RBBB with cardiac enzymes and troponins positive. She was getting multiple runs of ventricular tachycardia requiring DC shocks in view of worsening hemodynamics along with amiodarone. With dialysis K+ and acidosis was corrected but in spite of that patient was getting arrhythmias, hence balloon tip pacemaker was put and overdrive pacing was tried and with that incidence of arrhythmias had reduced. Her inotropes requirement was persistently increasing. Neurological deterioration was very rapid that within 24 hours patient was comatose, as there was no response to pain stimulus and deep tendon reflexes were absent with mute planters, however her pupils were reacting to light with ventilator trigger and cough reflex were present. Next day there was further worsening in neurological, clinical, hemodynamically as well as laboratory parameters as WBC — 40000, Hb- 13, platelets 77, SGOT 32489, SGPT- 6676, Bilirubin- 7.55, PT more than 2 min. Blood culture, swab of fluid from blisters and fluid culture showed no growth. Patient’s conditions rapidly deteriorated with increased inotropic requirement, intractable arrhythmias, and severe derangement in coagulation as well as worsening liver function test. In spite of aggressive management, she succumbed to her illness within 72 hours of ICU admission.
Discussion
Scleredema is usually a clinical diagnosis because of its typical skin manifestation but many a times requires skin biopsy for Definite diagnosis as microscopic features of the biopsy are characterized by thickening of the dermis due to enlarged collagen bundles in deep reticular dermis with clear spaces between them, filled often with mucin deposits, which are inconstant and not necessary for the diagnosis.3 There is some strong link reported in association with diabetes mellitus called scleredema diabeticorum, with isolated reported cases of monoclonal gammopathy, multiple myeloma in some patients of scleredema.
This unusual skin alignment, various treatment option and modalities has been tried like immunosuppressive drug such as systemic steroids, cyclosporine,4 methotrexate, or high-dose penicillin, or various modes of phototherapy, such as UVA1, narrow-band UVB, psoralen with ultraviolet light A (PUVA) either administered systemically or topically, 5 penicillamine, electron beam, and glycemic control with prostaglandin E1 (PGE1), have all been tried with limited success. In myeloma related scleredema, there are evidence of chemotherapy suppression for myeloma resulted in concomitant improvement of the skin disease and better prognosis.6 For patients with paraproteinemia, extracorporeal photopheresis has been used, but with variable results. Recently, multiple reports had described intravenous immunoglobulin (IVIg) therapy especially in postinfectious, diabetic, and monoclonal gammopathy–associated scleredema that were refractory to more standard therapies with better efficacy.7
In our patient diabetes was one of the predisposing risk factor. We have ruled out monoclonal gammopathy and myeloma in our case as bone marrow biopsy was suggestive of 4% plasma cells and reactive marrow. In our patient the most important key factor was high WBC count and LV dysfunction at time of admission. Hence, she was treated with IV daptomycin (as broad spectrum) to cover gram positive organism in view of suspicious cellulitis. There was severe LV dysfunction so possibility of sepsis related or associated myocarditis could not be ruled out. There was liver dysfunction with mild hepatomegaly and severe ascites. There was no feature of cirrhosis. Due to severe sepsis and refractory shock, there was acute kidney injury, with hyper kalmia and intractable arrhythmias and required urgent dialysis. All blood cultures, fluid from blisters and tissues from wound were negative for any organisms. There was poor response in spite of prompt treatment with antibiotics and steroids.8 So, this was a case of diabetes mellitus with sepsis and fulminant multiorgan dysfunction and the presenting feature was scleredema which unfortunately assumed a fulminant form. A review of the literature reveals very limited treatment guidelines especially of the non-fulminant form.
Conclusion
Appropriate prophylactic antibiotic therapy should be started in diabetes mellitus patients presenting with scleredema, because it’s a warning sign of preceding fulminant infection, although antibiotics do not appear to shorten the course of skin findings in scleredema.9 The role of steroids or immunosuppressants in fulminant conditions associated with sepsis still needs to be determined. Our case brought out the high mortality associated with Scleredema with comorbidities for which much need for further protocol and studies.