Introduction
Chyluria is an unusual manifestation of filariasis with milky white urine, due to passage of chyle into urine. It develops as a result of communication between the lymphatic system and the urinary system. In India, only in 2% of filariasis cases presents with this presentation.
Filariasis is a parasitic disease, most commonly caused by Wuchereria bancrofti (>90% cases). transmitted by bite of Aedes, Anopheles, Culex mosquitoes. Culex quinquefasciatus is the most important vector of W. bancrofti. The Adult worms of W. bancrofti reside in lymph nodes and lymphatics. The gravid female releases microfilariae which then enter general circulation through lymphatics. The disease can be seen as classical lymphatic filariasis or occult filariasis.1
This is a case of chronic urinary tract infection with hematuria followed by Chyluria as a presenting complaint. We also discuss here the approach to a common tropical problem of ‘white urine’ along with a review of relevant literature.
Case History
A 35-year-old male patient, Native of Uttar Pradesh came to Maharashtra in search of job and was staying here since last 5 years. Presently he is residing in Thane slum area since last 1½ years with 3 other males, working as a labourer in a private company. The patient was apparently alright 8 months back when he noticed white colour urine associated with burning micturition since 1 ½ months. He visited a hospital following the complaints and was admitted for 10days and given symptomatic treatment including antibiotics (Tab. Nitrofurantoin). The urine became clear post treatment and he remained symptom free for almost 2 months. However, the symptoms soon reappeared after completion of treatment.
After consulting various private practitioners, he did not get any relief. Then he visited to our hospital with complaints of Chyluria along with haematuria since last 7 days, associated with burning maturation, there was also h/o Minimal scrotal swelling left > right, mild fever and minimal abdominal pain. There was no history of inguinal Lymphadenopathy, pedal Oedema, diarrhoea / dysentery / constipation, groin pain / pelvic pain, weight loss or any past history of Diabetes / HTN /chronic illness, addiction / substance abuse or any family history of similar episode in past.
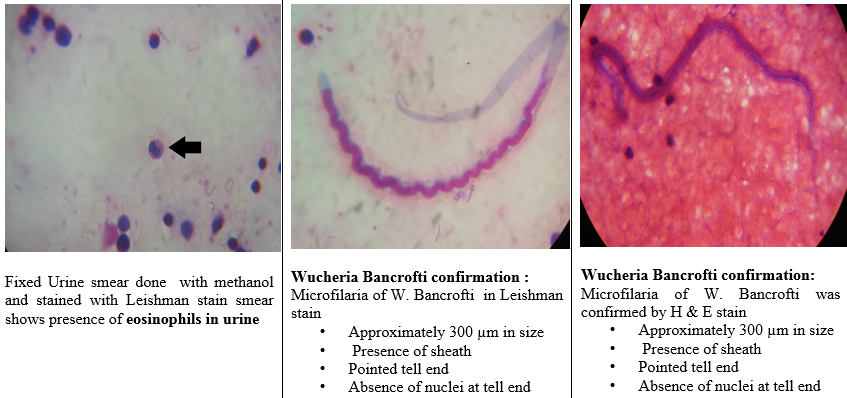
Figure 3
Urine sediment under 40X after centrifuging thesample at 300rpm.There was accidental detection of motile larva measuringaround 300 µm.Figure 3

Figure 4
USG abdomen, pelvis and genitourinary tractshowing Pre-aortic, Mesentric, Pelvic, Obturator lymph node not enlarged . Left inguinal lymph node was enlarged measuring 17mm in size. Bladder shows fine non-specific echo. Bilateral epididymo-orchitis with tuniculitis. Minimal hydrocele Left> Right. No e/o varicocele.

Table 1
Urine routine microscopy
Table 2
Treatment history
Table 3
Causes of chyluria
On examination, Vitals were normal, no evidence of lymphadenopathy including inguinal lymphadenopathy, minimal scrotal swelling Left > right, CVS: no abnormality detected, Respiratory system: no abnormality detected, Per Abdomen: no tenderness /No Organomegaly.
Investigations
Urine routine microscopy was performed (Table 1) and USG abdomen, pelvis and genitourinary tract done (Figure 2)
Nov 2018: Urine culture: Proteus mirabilis was isolated which was sensitive to Norfloxacin and treated with same drug.
The patient’s urine sample was centrifuged at 300rpm and motile larva was observed under 40X. (Figure 3 )
Urine wet mount and LPCB was prepared from the sample. (Figure 4)
DEC challenge test: It was conducted by administering DEC 2 tab stat before drawing out the peripheral blood. Peripheral blood smear was examined which confirmed microfilaria. (Figure 5)
Treatment given
DEC (100mg): ½ tab OD x 1 day, ½ tab BD x 1 day, 1 tab TDS x 21 days
Albendazole: 400mg for 12 days (Table 2)
Chyluria was not completely cleared till the last follow up. This is suggestive of lymphovenous fistula that needed further investigations which the patient refused to do. He was counselled for chyluria and advised for regular follow ups.
Discussion
Our patient presented with chyluria with chronic urinary tract infection and haematuria. After treatment also he complained of intermittent chyluria. In the endemic areas, up to 10% may be afflicted by filariasis.2 There are many causes of chyluria apart from filariasis (Table 1). Chyluria is a state of chronic lymphourinary reflux via fistulous communications secondary to lymphatic stasis caused by obstruction of the lymphatic flow. If the obstruction is between the intestinal lacteals and thoracic duct, the resulting cavernous malformation opens into the urinary system forming a lymphourinary fistula. Once such a fistula is formed, intermittent or continuous chyluria occurs.3, 4 (Table 3)
The natural history of chyluria is still unclear. Because spontaneous remission of chyluria may occur in 50% of patients, patients may not require treatment if the chyluria enters a long interval of remission without nutritional complications.5 However, in patients with persistent chyluria, malnutrition occurs from excessive urinary losses of lipids and protein. A specifically designed low-fat, high-protein diet supplemented with medium-chain triglycerides has been demonstrated to decrease the proteinuria, lipiduria and hematuria.6 The underlying cause should be treated for non-filarial chyluria. Filaricidal drugs are usually not helpful as the infection is burnt out by the time chyluria develops.
For patients with recurrent or persistent chyluria unresponsive to medical management, instillation of sclerosing solutions into the renal pelvis has an 80% success rate in achieving closure of the lymphatico- pelvic communication.7 Silver nitrate injection is a successful modality executed by urologists in India for recurrent and refractory chyluria. Povidone-iodine 0.2% is also considered to be as effective as 1% silver nitrate therapy. Anti-helminthic treatment should be considered besides providing definitive treatment for chyluria when microfilaria is found in urine samples.6
In India, cases have been reported from about 257 districts in 21 States/Union Territories and approx. 620 million people are at risk. The cases of filariasis have been recorded from Andhra Pradesh, Assam, Bihar, Chhattisgarh, Goa, Jharkhand, Karnataka, Gujarat, Kerala, Madhya Pradesh, Maharashtra, Orissa, Tamil Nadu, Uttar Pradesh, West Bengal, Pondicherry, Andaman & Nicobar Islands, Daman & Diu, Dadra & Nagar Haveli and Lakshadweep. Among these 21 states, 257 are endemic districts.8
However, the North-Western States/UTs namely Jammu & Kashmir, Himachal Pradesh, Punjab, Haryana, Chandigarh, Rajasthan, Delhi and Uttaranchal and North-Eastern States namely Sikkim, Arunachal Pradesh, Nagaland, Meghalaya, Mizoram, Manipur and Tripura are known to be free from indigenously acquired filarial infection.8
Prevention
Elimination of bancroftian filariasis is associated with a reduction of incidence of chyluria, as seen in some countries, such as Japan. In India, over 8 lakh cases of lymphoedema and 4 lakh cases of hydrocoele cases have been reported.8
The National Health Policy (2002) has set the goal of Elimination of Lymphatic Filariasis in India by 2015. Later extended to 2021. Twin pillar strategies of Mass Drug Administration (MDA) for interruption of transmission.8
Though initially single dose DEC was given as Mass Drug Administration (MDA), however; form 2018 Triple Drug Therapy (IDA) i.e. DEC + Albendazole + Ivermectin is launched initially in five selected districts. This is to be followed by annual Mass Drug Administration (MDA) of single dose of DEC (Diethylcarbamazine citrate) and Albendazole for 5 years or more to the eligible population (except pregnant women, children below 2 years of age and seriously ill persons) to interrupt transmission of the disease. The home based management of lymphoedema cases and up-scaling of hydrocele operations in identified CHCs/ District hospitals /medical colleges.8 Apart from MDA, decrease in the reservoir of parasite and environmental cleanliness to be approached to eliminate breeding sites of the Culex mosquitoes. The coverage of population with MDA should be above 80% persistently for 5-6 years which would reduce the microfilaria load in the community and thereby interrupt the transmission.
Conclusion
Government of India’s mission ‘Filaria free India by 2020 seem to be far from reality because many undiagnosed cases all across country, asymptomatic nature of disease, prolong incubation period and late manifestation of disease. Many are complacent when it comes to prevention; in part due to apathy towards the disease and the length of time it takes to manifest itself (8-10 years). Moreover, it is difficult to convince people to take tablets when they are in an asymptomatic stage every year for at least 5 years.
Hence, we do not have alternative apart from shifting Mass Drug administration program from 2 drugs (albendazole + DEC once year for 5 years) to 3 drug (Ivermectin, DEC and albendazole once year for 2 years) MDA strategy to become Filaria free India.