Background
An epidermoid cyst is a cutaneous cyst with an epithelial lining similar to the epidermis. The cyst lining produces keratin. The term "sebaceous cyst" is no longer appropriate because no sebaceous glands are present. Other words used to describe epidermoid cysts include inclusion cysts, epidermal inclusion cysts, epithelial cysts, keratin cysts, implantation dermoid, and traumatic or post-traumatic epidermoid inclusion cysts. An epidermoid cyst might occur because of the implantation of epidermal elements into the dermis during any trauma or surgery. We typically observe in farmers, factory workers, carpenters, and tailors because their occupation predisposes them to repeated mild hand trauma.1 The factors implicated in the formation of palmoplantar epidermoid cysts include HPV infection, UV exposure, and eccrine duct obstruction.2 Epidermoid cysts are more common in the elderly and patients taking medications like BRAF inhibitors such as imiquimod and cyclosporine, especially their face.3
Case Description
A 66-year right-hand dominant male laborer reported to our academic institution with swelling on the palmar aspect of the right middle finger. He complained about pain and the inability to work at his job for the past four months. He had first observed the swelling seven years ago after trauma due to hammer and chisel. It increased in size over the years but posed a significant problem from the past four months. The clinical exam revealed a 2.5 cm x 2.5 centimeters, smooth, tender, immobile, non-compressible firm swelling on the volar aspect of the right middle finger overlying the middle phalanx (Figure 1, Figure 2). There was no evidence of the central punctum (that is, the clogged orifice of the pilosebaceous follicle). We suspected an epidermoid cyst because of a history of trauma. The differentials included giant cell tumor of the tendon, Pilar cyst, foreign body granuloma, hemangioma, ganglion, and lipoma. We did the X-ray to rule out any foreign body because of trauma (Figure 3).
A finger tourniquet made from a glove was used to prevent bleeding. We performed the excision of swelling under a wrist block. Before making the incision, we performed aspiration, which resulted in a dry aspirate. The cyst burst open during dissection, resulting in spillage of cheesy material. (Figure 4, Figure 5).
Figure 1
Cyst overlying the middle phalanx causing difficulty to perform the activities of daily living.

Figure 2
Cyst overlying the middle phalanx causing difficulty to perform the activities of daily living.

Figure 6
Histopathology slide showing stratified squamous epithelium, with granular layer (blue) and giant cells adjacent to the granular layer and keratin.
Figure 7
Stratified squamous epithelium along with granular layer, no sebaceous glands are seen on the histopathology exam.
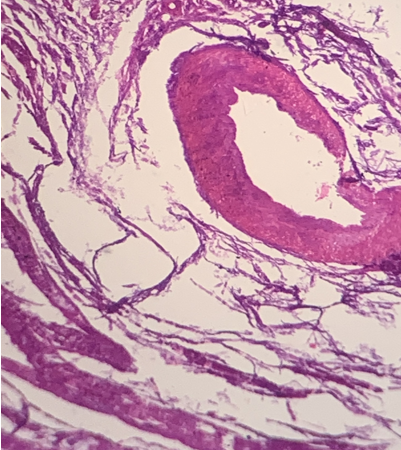
The histology confirmed the diagnosis (Figure 6, Figure 7). Histopathology showed a lining of stratified squamous epithelium with a granular layer containing keratin arranged in a lamellated pattern. (Image) Other findings included the giant cells, new vessel formation, and absence of rete ridges.
After surgery, the patient’s range of motion improved significantly. We did the sutures removal after ten days, and the follow-up was unremarkable.
Discussion
Epidermoid cysts form by the proliferation of epidermal cells within a specific dermal area. The lipid makeup of the epidermal cyst is identical to that of the epidermis. These cysts contain cytokeratin 1 and 10. The cytokeratins are formed in the suprabasal layers of the epidermis and expressed within the cysts. The origin of this epidermis is almost invariably the hair follicle’s infundibulum.4 Males are two times more likely than females to have epidermal cysts. Although Epidermoid cysts can occur at any age, they are most common in the third and fourth decades of existence. The most often affected location (32 percent, 33/103) is the head and neck, followed by the lower limb (26.2 percent, 27/103), the back (19.4 percent, 20/103), and the upper limb (9.7 percent, 10/103).5, 2 Epidermoid inclusion cysts also emerge from deeper tissues, such as tendon and phalangeal bones in isolated cases. Phalangeal lesions most frequently affect the distal phalanx and present with variable degrees of pain, edema, nail deformity, and erythema on rare occasions. Several authors have proposed the development of a phalangeal cyst because of direct traumatic implantation of epidermal fragments into bone or migration of a portion insertion of the nail bed into the bone.4 In contrast to cysts at other locations, the palmoplantar cysts are not fluctuating and are immobile because of the thickness of the skin concerning anatomical areas.
Most epidermoid cysts are benign lesions but might become malignant in a rare case. A history of associated trauma and clinical examination is usually adequate to confirm the diagnosis of epidermoid inclusion cysts because they are frequently site specific. Imaging studies do not result in a conclusive diagnosis, but we recommend them as part of a comprehensive assessment. The most common type of diagnostic modality used to diagnose the epidermoid cyst is the X-rays. Although ultrasonography can be done, it only infrequently provides a conclusive diagnosis. CT scan and MRI are helpful techniques in defining the architecture of soft tissue cancers, but this is rarely required to guide treatment. Fine-needle aspiration cytology (FNAC) is helpful if the amount of keratin or sebaceous material obtained is adequate to perform the cytological examination. Histopathologic findings of a cystic lesion are used to make the final diagnosis. The cyst wall lining comprises stratified squamous epithelium and contains lamellated keratin. We may see calcification in cysts that have been there for a long period, the inflammatory response may or may not be present.
We must distinguish hand epidermoid inclusion cysts from ganglions, tendon sheath giant cell tumors, and lipomas, as well as bony and arthropathic swellings. Surgical therapy is only required for symptomatic cysts because most hand dermoid cysts are benign. The sudden growth in size frequently indicates complications such as rupture, infection, or malignant transformation. When hand function is compromised, we must excise the cyst. We can perform surgery under a brachial plexus or wrist block. Either a pneumatic tourniquet put across the arm or a finger tourniquet tied near the MCP joint can minimize the blood loss during the procedure.
Clinical significance
Here, we demonstrate a novel location for an epidermal inclusion cyst and the value of histopathologic examination. We also stress the importance of thorough inspection of the epithelium surrounding the cyst for complete removal of the capsule to prevent recurrence or omission of any other pathology.
Ethical Statement
We described the technique to the patient in her native language and obtained her approval to submit the article and accompanying photographs for publication.




