Introduction
Schwannomas are tumors of nerve sheath derived from Schwann cells of the peripheral, cranial or autonomic nerves. It is also known as neurilemmoma or neurinoma and was first described by Verocay in 1908. The Schwannomas of head and neck region are solitary, firm in consistency, homogenous, mostly benign, slow growing, well-defined and encapsulated tumours.1 Approximately 25-40% of the total schwannomas, are head and neck Schwannomas, they may originate from nerve sheath of the peripheral, cranial or autonomic nerves. Submandibular region Schwannomas are rare form of head and neck schwammomas.2 These tumours are noticed as slow growing swelling or mass in Submandibular region, they are asymptomatic with no age or sex predilection.3 Schwannomas are of long duration, because they grow deep and are painless and no surface changes in the overlying skin are observed at the time of the presentation however; rarely do they show a rapid course.4 In about 10 - 40% of schwannomas the nerve of origin can’t be identified.5 On histopathological examination two types of schwannoma cells: Antoni type A and Antoni type B can be demonstrated.6 We present a rare case of a right submandibular region schwannoma of a 25-year-old woman who presented with a painless, insidious, asymptomatic, and progressive swelling in the right submandibular region.
Case Report
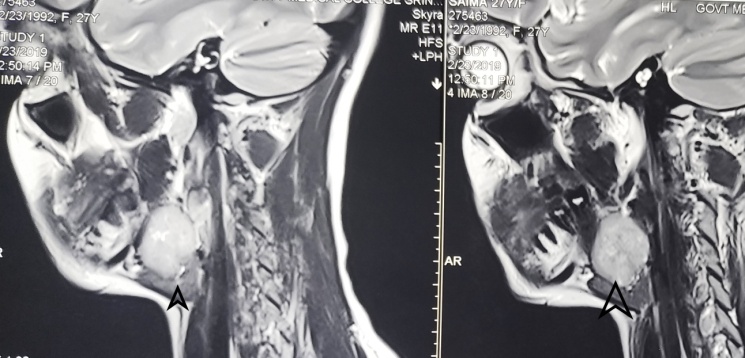
A 25-year-old woman reported to our department (Department of Oral Medicine and Radiology) with a painless mass on the right side of his neck. She noticed the swelling four months ago, the swelling was progressive in size (Figure 1). There was no history of overlying skin changes, ulceration, or discharge. She did not notice any other swelling. The patient reported no history of anorexia, weight change, or night sweats. No recent history of fever or prior history of URTI, nor there was pain or increase in size of swelling during eating food. No history of difficulty in respiration. No similar past or family history. Her past medical and surgical history had no relevant or significant finding.
Physical examination on the right side of his neck revealed a mass of approximately 3cm×2cm in its greatest diameter, the surface was smooth and no signs of ulceration, pus drainage or colour change was seen, on the right side of the submandibular region. On palpation the swelling was non-tender, firm in consistency, homogenous in texture, non-pulsatile, non-fluctuant, mobile, and was not attached to the underlying or surrounding structures. On auscultation no bruit present. Otherwise, examination of the head and neck had no significant finding. No regional lymphadenitis was detected. The examination of cranial nerves was normal.
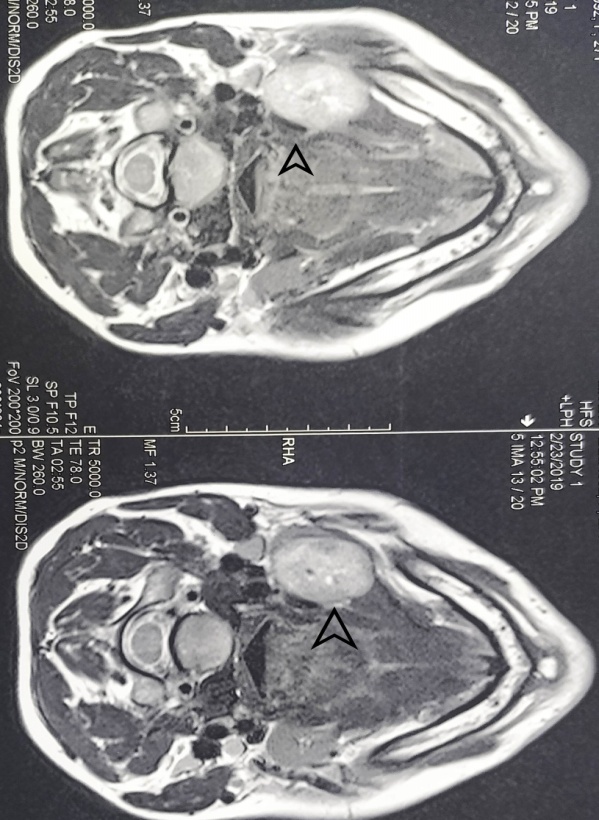
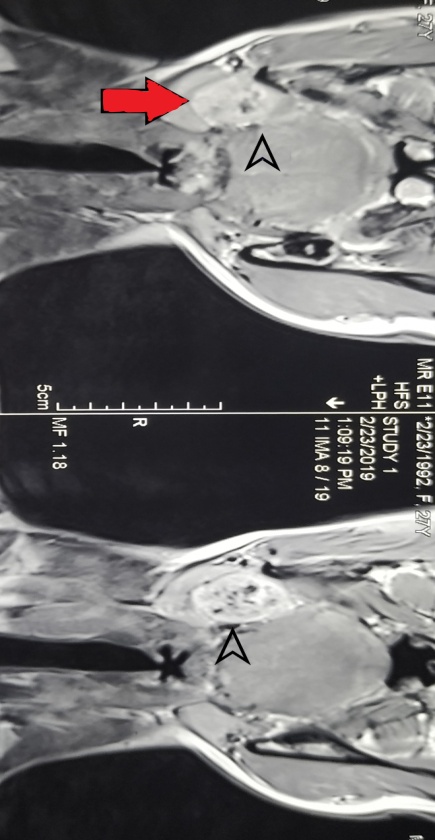
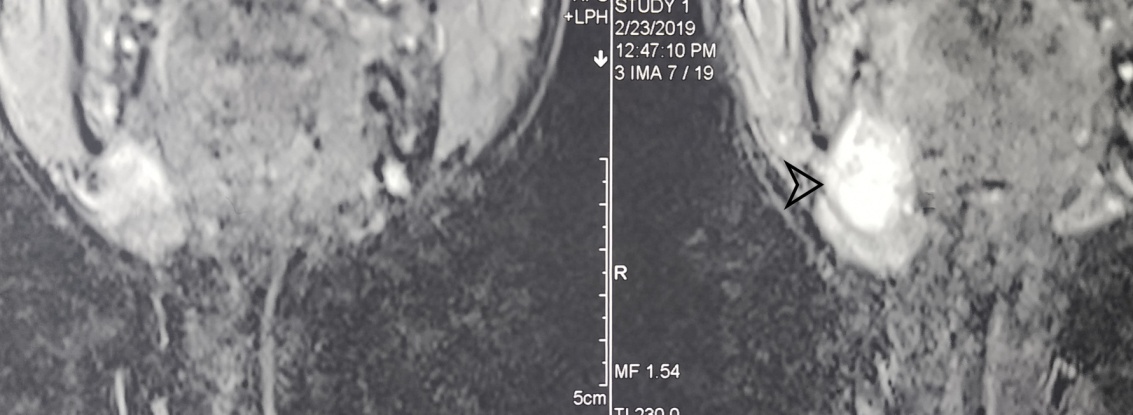
An ultrasound revealed well circumscribed hypoechoic solid lesion with internal vascularity with in submandibular triangle displacing and compressing the submandibular gland but is separate from submandibular gland (Figure 2). No cervical lymphadenopathy seen. USG guided FNAC was inconclusive. CE MRI revealed a well defined, encapsulated solid lesion measuring 3.2cm×2.2cm×2cm in right submandibular space and invaginating right submandibular gland. The lesion on T1 weighted MRI images exhibits homogenous isointensity and on T2 weighted MRI images exhibits heterogenous hyperintensity, on contrast enhanced T1 MRI images it exhibits salt and pepper type of enhancement. Lesion exhibited mild diffusion restriction on periphery (Figure 3, Figure 4, Figure 5, Figure 6). On the basis of above clinical and imaging findings the lesion was suspected to be a tumour of salivary gland or neurogenic. The patient was referred to surgical oncology department for surgical evaluation and excision. Complete excision of the gland was done and HPE reports came out to be schwannoma of right Submandibular region. Patient was relieved of previous symptoms post-operatively.
Discussion
We report a case of Schwannoma of right side Submandibular region in a 25-year-old female with no significant dental, personal or medical history. Schwannomas are slowly progressive benign lesions, the patient presents with a mass or swelling that is growing in size slowly. The lesions at the time of presentation are usually painless, non-tender, smooth surfaced swelling that are deep under the mucosa with no changes in the overlying skin. The lesions are noticed after they have grown in size to displace the surrounding structures.7 The lesion may however become symptomatic due to secondary infection or at advanced stages of the disease giving rise to pain and neurological symptoms, because the tumor is smooth and encapsulated that grows slowly over a period of time.8 The most common location of Schwannomas in the head and neck region is the tongue.9 Schwannoma was described first in 1908 by Verocay, commonly occurs between 30 and 50 years of age and in our case it is a 25-year old.10
Our case presented with a slowly progressing, solitary and painless, right submandibular swelling with a good post-operative prognosis which is clinically comparable with the works done by Ho CF et al.,11 Satish Kumar Ranjan et al.12 and Gaffar Aslan et al.13 Plain radiography is not useful for reaching out to a diagnosis of schwannoma. Ultrasound examination reveals a well circumscribed and hypoechoic mass. FNAC is not always conclusive as erroneous results indicating pleomorphic adenoma might be reported. The Diagnostic investigations used for Schwannomas are computed tomography (CT), magnetic resonance imaging (MRI), ultrasound scan and Fine Needle Aspiration Cytology (FNAC). Magnetic resonance imaging (MRI) is the best choice in detecting the extent and margins of the tumor as they invaginate and compress the surrounding structures and correlates well with the operative findings.14 The diagnosis of the schwannoma was suspected because of the MRI appearance of the lesion exhibiting hyperintensity on and salt and pepper type of enhancement. The lesion exhibited mild diffusion restriction on periphery and the presence of intratumoral vessels on MRI, and the capsule of the tumor exhibited high attenuation and delineation from the displaced submandibular salivary gland. The MR images in our case showed homogeneous isointensity on T1 weighted images, and on T2 weighted showed heterogeneous hypointensity, and heterogeneous enhancement on contrast-enhanced T1-WI. The capsule appeared clear and showed hypointensity on T2 weighted images. The imaging characteristics of the lesion are suggestive of neurogenic origin.15 Biswas et al. in his 10 years of experience regarding extracranial head and neck schwannomas reported only 6 percent of patients could have been diagnosed preoperatively on the basis of history, clinical findings, CT and MRI scans, and Fine Needle Aspiration Cytology (FNAC).16 The MR images of Schwannomas have specific MRI properties, including specific signs (split-fat sign, fascicular sign, target sign) and signal patterns (that is, isointense T1 signal; hyperintense heterogeneous T2 signal). The diagnosis of Schwannoma is confirmed histopathologically by showing the presence of Antoni type A cells and Antoni type B cells, nuclear palisading, whirling of cells and Verocay bodies.17 We believe this tumor to have originated from autonomic nerve of the submandibular gland.
Conclusion
History and clinical examination do not help to reach at clinical diagnosis as they are similar for pleomorphic adenoma and schwannoma. FNAC is also many a times inconclusive. MR findings are not specific. It is HPE and IHC that confirms the diagnosis. Submandibular gland schwannomas run a benign course and excision is the definitive treatment.