Introduction
Cystic lesions developing from the salivary glands are commonly known as "mucoceles", these lesions develop mostly in relation to the minor salivary glands and rarely, in relation to the major salivary glands. Mucoceles are of two types: Mucous retention cyst and Mucous extravasation cyst. Mucous retention cyst results from obstruction to the duct of the minor salivary gland because of a sialolith, periductal scar, or impinging tumour, which leads to accumulation of saliva within the gland or its duct, thereby causing its expansion. Whereas Mucous extravasation cyst develops as a result of mechanical trauma to the salivary gland excretory duct, resulting in its severance. A ranula is a form of mucous extravasation cyst which commonly occurs on the floor of the mouth.
The term “Ranula” originates from the Latin word “Rana” which means frog since the swelling resembles the translucent underbelly of the frog.1 Ranulas usually remain asymptomatic or present with a painless bluish fluctuant swelling commonly occurring on the floor of the mouth. Ranulas are characteristically large (>2cm) and appear as tensed dome-shaped vesicles.2 Deep-seated lesions have normally appeared overlying mucosa and in Superficial lesions, the mucosa may have a translucent bluish colour.1 The majority of these lesions result from extravasation of saliva secondary to trauma; however, their occurrence in young children may indicate dysgenetic development of the sublingual gland duct system.3 This article presents a case report of Ranula in a 47 years old female patient treated with the excision of the Ranula. Follow-up revealed no recurrence.
Case Report
A 47-year-old female patient reported to the department of Oral and Maxillofacial Surgery with a chief complaint of swelling below the tongue on the left side for the past 2 months.
History revealed that the swelling which was initially of a peanut size has gradually increased and attained the present size. The patient gave a history of difficulty in mastication and speech. Past dental history reveals that the patient got her tooth # 33, 34, 35 extracted 22 days back.
Family history and personal history and previous history of swelling were not contributory. On systemic evaluation, there was no significant abnormality detected. On Extra oral examination, there were no regional lymph nodes palpable and there was no evidence of any other neck swelling. On examination, general condition was normal and vital signs were stable.
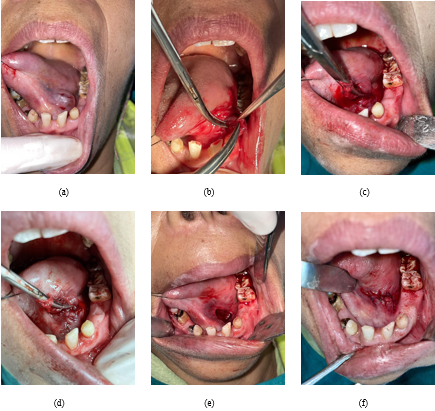
Intraoral examination showed solitary with a slight bluish tinge, well-circumscribed swelling measuring about 2 X 1 cm in the floor of the mouth on the right side extending from midline to lingual side of the alveolar ridge, anteriorly up to the mesial aspect of tooth #33; posteriorly up to tooth #34,35 regions as shown in Figure 1.
The swelling was localized, non-tender, and soft and cystic in consistency. The swelling was of the same colour as adjacent mucosa with a slight bluish tinge and no discharge was elicited.
Correlating with the history and clinical findings, the case was provisionally diagnosed as Ranula. Radiographic examination with mandibular occlusal radiograph showed no abnormal changes.
Ultrasonographic evaluation of the swelling revealed a well-delineated cystic lesion measuring approximately 18.3 X 14.7 mm is seen in the submental location left of the midline. No septations seen within it. In addition, an Ultrasound of the thyroid revealed that both submandibular glands were normal. A few subcentimeter-sized lymph nodes were seen in bilateral submandibular regions with the largest measuring approximately 6.5 mm in short axis diameter. They show fatty hilum.
The right lobe and isthmus of the thyroid gland are normal in size and echotexture. The left lobe of the thyroid shows a solid cystic mass measuring approximately 18.6 x 14.3 mm. Low-level echoes are seen in cystic areas with few echogenic foci showing comet tail artifacts. Bilateral neck vessels are normal.
After a preoperative investigation which was within normal limits, excision of Ranula was carried out under Local Anaesthesia and was subjected to histo-pathological examinations which revealed highly inflamed stroma with some areas showing epithelium. Connective tissues show granulation tissue cells, numerous lymphocytes, and plasma cells forming the central cavity. In some areas, minor salivary glands were seen. Sutures were removed after 7 days and the patient was followed up every week.
Discussion
A ranula is a form of mucous extravasation cyst, which specifically occurs on the floor of the mouth in association with the ducts of the sublingual gland; the ducts of Rivinus. The name is derived from the Latin word “Rana”, meaning frog, since the swelling resembles the translucent underbelly of the frog.1 The ranula appears as a blue, dome-shaped, soft, cystic fluctuant swelling on the floor of the mouth which gives brilliant transillumination.
The majority of these lesions result from extravasation of saliva secondary to trauma; however, their occurrence in young children may indicate dysgenetic development of the sublingual gland duct system.
The occurrence of Ranula is rare and accounts for 6% of all oral sialoceles. Even though the prevalence is 0.2/1000 cases, less than 10% are true cysts. The reported male-to-female ratio is 1:1.3, without significant side preference. These lesions commonly occur unilaterally and rarely bilaterally. Ranula usually occurs in children and young adults with a peak incidence in the second decade of life. A study of series recorded an age range of 5 months-39 years which is at variance with a study that recorded 3-61 years.4
Clinically, it presents as a solitary, well-circumscribed, soft, bluish swelling covered by a thin layer of epithelium. Deeper lesions may be normal in colour.
An unusual clinical variant, the plunging or cervical ranula occurs when the fluid pressure of mucin of the deeper lesions dissects through the mylohyoid muscle into the submandibular space and causes neck swelling. The diagnosis of plunging Ranula is confirmed by cross fluctuation test, demonstrated by bi-digital palpitation. Ranulas can develop into large masses ranging from many centimetres in diameter, fill the floor of the mouth, and elevate the tongue.
The diagnosis of Ranula is based principally on clinical examination. Radiological methods such as high-resolution Ultrasonography are used to identify cystic lesions. In the case of Ranula, an Ultrasonographic evaluation of the swelling revealed a well-delineated cystic lesion measuring approximately 18.3 X 14.7 mm is seen in the submental location left of the midline. No septations seen within it. In addition, an Ultrasound of the thyroid revealed that both submandibular glands were normal. A few subcentimeter-sized lymph nodes were seen in bilateral submandibular regions with the largest measuring approximately 6.5 mm in short axis diameter. They show fatty hilum.
The right lobe and isthmus of the thyroid gland are normal in size and echotexture. The left lobe of the thyroid shows a solid cystic mass measuring approximately 18.6 x 14.3 mm. Low-level echoes were seen in cystic areas with few echogenic foci showing comet tail artifacts.
Bilateral neck vessels were normal. Imaging studies like computed tomography or MRI are done to confirm any extension of the swelling prior to surgery or when the diagnosis is unclear. Radio-graphically the presence of the “tail sign” is pathognomonic for the plunging Ranula.5, 6, 7 This tail is due to extension behind the mylohyoid muscle and confirms the ranula to arise from the sublingual gland.8
Clinics' differential diagnoses of the floor of the mouth swellings include sublingual dermoid cyst, salivary gland tumours, benign mesenchymal neoplasms, submandibular salivary gland sialadenitis, Lipoma, and haemangioma. A sublingual dermoid cyst is a thick-walled cyst, whitish in colour and not transilluminant. Salivary gland neoplasms like Adenoid cystic carcinoma. Mucoepidermoid carcinoma usually occurs on the floor of the mouth and is associated with pain and bleeding.9 Lipomas occur rarely intraoral usually occurring in the buccal mucosa, the floor of the mouth, and tongue, and clinically show yellowish mass with encapsulation.9 Hemangiomas are developmental lesions clinically seen as deep red colours which show compressibility and blanching on palpation. Mucoceles are usually seen on the lower lips with a history of lip biting and smaller size as compared to that of Ranula. If a mucocele appears in the alveolar mucosa, an eruption cyst or gingival cyst should be included in the differential diagnosis. Plunging ranulas, thymic cysts, and cystic hygroma might be considered.
Histo-pathologically, a well-circum-scribed cavity lined by granulation tissue contains free mucin. The mucin and granulation tissue are infiltrated by large numbers of neutrophils, macrophages, lymphocytes, and occasionally plasma cells. The adjacent salivary gland whose duct was transected shows ductal dilatation, scar, chronic inflammatory cells, and acinar degeneration. In this case, histo-pathology revealed a highly inflamed stroma with some areas showing epithelium. Connective tissues show granulation tissue cells, numerous lymphocytes, and plasma cells forming the central cavity. In some areas, minor salivary glands were seen.
The lesion has been treated in a variety of ways ranging from simple aspiration to complete or partial excision of the ranula and/or the sublingual salivary gland, at times involving the submandibular salivary gland. They include marsupialization, dissection, cryotherapy, sclerotherapy, hydro-dissection, and LASER ablation. The sclerotherapy employs bleomycin-antineoplastic antibiotic of Streptomyces verticillus-OK-432 (Picibanil), a lyophilized mixture of a low virulent strain of Streptococcus pyogenes incubated with benzylpenicillin, that has been found to produce good effect.10, 11
The recurrence rate varies according to the procedure performed. Crysdale et al.12 reported that the recurrence rate was 100% in cases with incision and drainage, 61% in cases of simple marsupialization, and 0% in cases of excision of the ranula with or without sublingual gland excision. In this case excision of Ranula was carried out under Local Anaesthesia and patient follow-up was done for 3 months with no recurrence.
Conclusion
We concluded that Intraoral and Plunging Ranulas are trauma- associated mucous extravasation cysts occurring in the floor of the mouth and in the submandibular region respectively, both originating from the ducts of sublingual salivary glands. With the current knowledge of pathophysiologic basis, excision of Ranula by a specialist Oral and Maxillofacial surgeon is a key for successful results.