Introduction
Neuroendocrine neoplasms (NENs), defined as epithelial neoplasms with predominant neuroendocrine differentiation arising from enterochromaffin cells. Various terms for the epithelial NENs were carcinoid, argentaffinoma, APUDoma, small cell carcinoma, islet cell tumor, medullary thyroid carcinoma, Merkel cell tumor, neuroendocrine tumor. The neuroendocrine tumors are rare slow-growing tumors with distinct histological, biological, and clinical characteristics. NENs can develop in almost all organs of the body. Ileal Neuroendocrine Tumor (NET) are the most frequent site of gastrointestinal NET followed by the rectum, appendix.1 Although the nomenclature of NENs have been complex, the histopathological diagnosis and classification of NET have improved considerably over the last decades. Neuroendocrine tumors were first described by Langhans in 1867.2 In 1907, Oberndofer first described these tumors arising from the epithelial cells in small intestine as “carcinoid”.3 Neuroendocrine tumors previously called carcinoid tumors are neoplasms of enterochromaffin or neuroendocrine cell origin. In 2000, the World Health Organization classification replaced “carcinoid” with the terms neuroendocrine tumors and neuroendocrine carcinomas to describe gastrointestinal neoplasms originating from the diffuse system of neuroendocrine cells.4
The classifications of Neuroendocrine tumors (NETs) by the WHO 2010 classification is based on histological parameters and the proliferative index. NETs are graded as low (G1), intermediate (G2), and high (G3) grade i.e neuroendocrine carcinoma (NEC). The high-grade carcinomas (NEC) resemble small cell carcinoma or large cell NEC of the lung.5
The new category of G3 neuroendocrine tumor (NET) was first introduced in the 2017 WHO classification of pancreatic tumors and later extended to all gastrointestinal NENs in 2019 WHO (G1, G2 and G3 well-differentiated NEN and others).6
Herewith we present rare case of well-differentiated neuroendocrine tumor, NET, G2, Intermediate grade of ileum.
Case Report
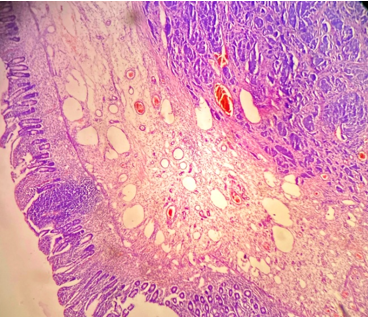
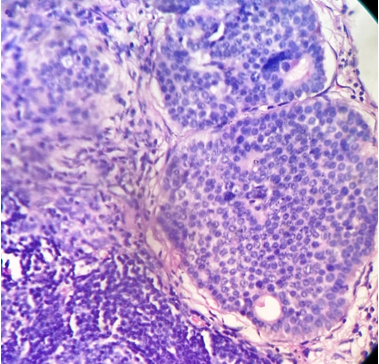
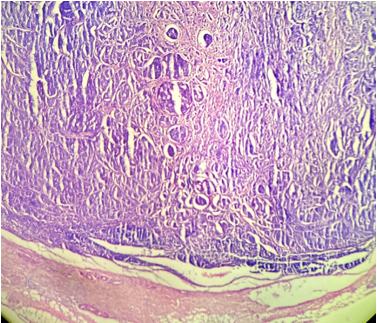
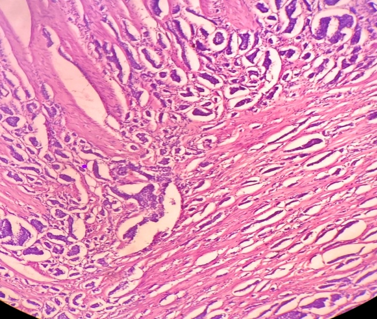
A 65-year old male came to the surgery unit with complaints of recurrent abdominal pain since 1 year which had increased in last 7 days. The pain was insidious in onset and gradually increased, was not relieved by medications. He also complained of vomiting which was watery in nature, loss of appetite and diarrhea. P/A examination reveals tenderness and lower abdominal swelling. On ultrasonography finding impression of small bowel mass lesion suggestive of ileac carcinoid tumor with ischemic bowel disease was given. On CT scan abdomen and pelvis showed a mass located at the ileum and was about 10 cm above the ileocecal valve, and it seems that luminal narrowing causing obstruction in the 3cm segment. The wall was oedematous, thickned. Mass was well-defined, round, hetergenous, enhancing, measuring 2.6 x1.6x1.2 cm. The mild ascitis was noted. Rest all organs were normal. In areas few isodense plaque like arterial enhancing lesions in superior mesenntric artery were noted. On radioimaging finding impression was mid small bowel loops mass lesion indicates neuroendocrine tumor (carcinoid) was given. The surgical resection of ileum with mass and mesenteric nodes were done. Grossly, we received a specimen of ileum, totally measuring 38 cm in length. External surface of which is congested with focal area of adhesion. The mid segment showed constriction and distal segment showed ischemic changes. On cut open ileum mid segment showed multiple, irregular mucosal thickenings with foci of ulceration. The submocosa showed single, circumscribed, round tumor measuring 3 x2.5x1.5 cm extending up to serosa with variable size tiny nodules around it. Cut section of tumor was yellowish, tan, well circumscribed and solid.(Figure 1, Figure 2) The surrounding intestinal wall showed constriction. The enlaged mesenteric lymph node was identified. On cut section lymph nodes were yellow, grey white, firm, friable material. The microscopic examination ileum showed a tumor composed of uniform, round cells having to oval nuclei with salt pepper chromatin. Tumor cells are arranged in trabecular, nests, ribbons and in areas pseudo glandular pattern. (Figure 3, Figure 4, Figure 5) Mitotic activity was noted (4/10 high power field). Tumor is seen extending from submucosa upto serosa. Areas of congestion and moderate inflammatory cell infiltrate is noted. The lymphovascular invasion was present. Mesenteric lymph nodes were involved by tumor.(Figure 6) On histopathology reported as well-differentiated neuroendocrine tumors NET,G2, intermediate grade ileum. The immunohistochemical stain were positive for synaptophysin, chromogranin A. The a Ki-67 expression was <1%. Patient was kept on regular follow up and responded well to treatment.
Figure 2
On gross ileum cut openshowing single, yellowish- tan, circumscribed ,round mass with irregular mucosal thickenings with ulceration.

Figure 4
Tumor composed of uniform neoplastic cells arranged in solid nests, tabeculae with invasion in muscle layer. (H& E stain, ×200).
Discussion
Neuroendocrine tumors (NETs) represent a rare, slow-growing neoplasm. NETs are a neoplasms that arise from neuroendocrine cells and express neural markers, such as synaptophysin or chromogranin A. In last few decades gastrointestinal neuroendocrine tumors (NETs) are being diagnosed more frequently. The latest figures from the US’s Surveillance Epidemiology and End Results (SEER) Register show that in the past 35 years, the number of neuroendocrine tumors/carcinomas of the small intestine has increased 300%-500%. The reasons may be due to earlier detection with the increased use of endoscopy, newer histopathological technics to diagnosis etc. According to SEER Program, the age-adjusted annual incidence of NETs arising from jejunum and ileum is 0.67 per lakh.7 The most common locations for these tumors along the GI tract are the esophagus and the large intestine, but they can arise anywhere. The behaviour of NETs differs by anatomic site and is very heterogeneous.8, 9 The NET-G1 are relatively indolent.
In our case patient presented with complaints of recurrent abdominal pain with signs of bowel obstruction. Clinically initial presentations are with vague abdominal pain, cramping, bloating, diarrhea gastrointestinal bleeding, flushing, sweating, etc. Some cases signs of bowel obstruction, perforation were noted. The ileocolonoscopy used to detect ileal NETs, but with the evolution of diagnostic tools like capsule enteroscopy and balloon-assisted enteroscopy were more helpful for diagnosis.
It is mandatory in the pathology report to specify the grade or differentiation of the tumor. The histological parameters such as tumor size, mention about tumor unifocal or multifocal, mitotic count, lymphatic or vascular invasion, nodes involvement, metastasis, etc. The proliferative index Ki-67 is important in the patients management and prognosis.The Neuroendocrine tumors are graded as a) grade 1: as, low grade, having < 2 mitoses/2 mm2, Ki67 index: < 3% b)grade 2, as intermediate grade having 2 - 20 mitoses/2 mm2, Ki67 index: 3 - 20% and c)grade 3, as high grade having > 20 mitoses/2 mm2, Ki67 index: > 20%10
It is noted that depending on tumor size, the rate of loco regional lymph node metastases varies. However, lymph node metastases may be observed in ileal NETs as small as in 5 mm tumor size. The peritoneal seeding, distant metastases occurs in 19%-64% of patients.11
The majority of neuroendocrine tumors of the small intestine are low-grade G1 or G2 shows slow local growth and usually have a low proliferation rate Ki-67 ≤ 2%. These are frequently diagnosed at an advanced stage of metastatic disease. While the NEC are considered extremely aggressive, with a bad prognosis. The metastasis is frequently noted in the liver, lymph nodes, lungs, bones, etc. Miller HC observed that the patients with NET showed metastasis in 46.1% of the G1 cases, 77.8% of the G2 cases and 100% of the G3 cases.12
The neuroendocrine cells express neural markers, such as synaptophysin or chromogranin A. The plasma chromogranin A is elevated in 60%-100% of patients with NET, with a sensitivity and specificity of 70% to 100%.13 Other markers like Neuron specific enolase, PGP9.5 and CD56 are sensitive but not specific. The small bowel NETs as a genomically stable cancer, with low mutation rates. The genes, most of which were known for being cancer genes included FGFR2, MEN1, HOOK3, EZH2, MLF1, CARD11, VHL, NONO, and SMAD1. etc.14
Bowel resection along with lymph node dissection is usually performed. For early detected tumor, surgical excision gives good result. The surgical treatment for neuroendocrine tumors is curative in stages I-III or palliative in stage IV in an attempt to avoid local complications of bowel obstruction and ischemia of the small bowel.15, 16, 17 The recent treatment of NETs includes novel drugs such as somatostatin analogs, somatostatin receptor-coupled radioligands, molecular therapies and advace technics in surgery with locoregional resections depeding on tumor type, grade and stage.18
In our case the lymph vascular invasion and mesenteric lymph nodes were involved by tumor. Patient was kept on regular follow up and responded well to treatment. It is observed that, even small size NETs within the ileum have a high tendency of metastatic spread to the regional lymph nodes.16 For the gastrointestinal tract NET, if the tumor has spread to nearby tissue or the regional lymph nodes, the 5-year survival rate is 95%, while if distant metastasis is present then the survival rate is 67%.19 The overall prognosis in well and moderately differentiated NETs are relatively good as tumor is less aggressive.
Conclusion
Ileum NETs are diagnosed very rarely. The behaviour of NETs differs by anatomic site. Herewith the review and presention of rare case of well-differentiated neuroendocrine tumors, NET, G2, intermediate grade ileum for its clinical, radio imaging, pathological features and management was done.