Introduction
Adenomatoid odontogenic tumor (AOT) is a rare encapsulated benign tumor arising from the odontogenic epithelium which is usually associated with an indolent behaviour. This neoplasm is characterized by the peculiar histopathological findings of rosette or duct like structures. The term AOT was purposed by Philipsen and Birn in the 1969 WHO classification.1, 2 Before this nomenclature, this neoplasm traversed a long and dynamic journey of nomenclatures with the first one being called as “Cystic Adamantinoma” described by Harbitz. The irrefutable evidence supporting this tumor to be cystic in nature has been the point of discussion since long. Some authors like Ide et al. advocate the AOT should be identified as an Adenomatoid Odontogenic cyst (AOC), however, another school of authors justifies that it is correctly classified as a tumor. The evidence supporting both schools of thoughts are available but in our opinion this neoplasm behaves like a true solid tumor with foci of cystic degeneration and should be continued to be treated as a tumor.2, 3, 4
The latest WHO classification 5th edition places AOT in the Benign epithelial odontogenic tumor category and defines it as a “benign encapsulated epithelial odontogenic tumour that contains rosette or duct-like structures and has an indolent behaviour”.5
In this article we discuss a case of AOT in 28 year old female involving anterior maxilla with emphasis on the characteristic histopathological features.
Case Report
A 28 year old female presented to the out patient department (OPD) of a tertiary care hospital with the chief complaint of a swelling on upper lip along with slight mobility of teeth in that region since few months. On extra-oral examination, the upper lip on the right side was slightly raised. Intra-oral examination revealed a firm to hard swelling on the right side of anterior maxillary region involving lateral incisor to first molar region. The associated teeth were grade 1 mobile and the overlying mucosa was congested and slightly tender on palpation. An orthopantomogram (OPG) was advised which revealed a well defined corticated unilocular radiolucency extending from maxillary second incisor medially to second molar laterally and superiorly reaching and obscuring the floor of maxillary sinus. The lesion was displacing and resorbing the apical third of the roots of maxillary first and second premolars and first molar (Figure 1 A). Associated both premolars were tender on percussion. The clinico-radiological findings were favoring a benign lesion possibly benign odontogenic tumors like Ameloblastoma or Adenomatoid odontogenic tumor. Considering the slow growing nature and well delineated radiographic presentation of the lesion, a complete excision of the lesion was planned. Patient underwent surgical excision of the tumor by raising a flap and the tumor had caused thinning of the cortices (Figure 1 B). The excised specimen was submitted to the pathology department for histopathological examination. The specimen submitted consisted of a rounded grey white to grey brown soft tissue piece encasing three teeth- maxillary canine and first and second premolars. Cut section showed solid areas with focal cystic change along with areas of hemorrhage (Figure 2 A). The roots of both premolars were resorbed upto the cervical portion of the roots. Multiple sections of the specimen were submitted for microscopic examination.
Figure 1
A): OPG reveals a well circumscribed unilocularradiolucency in anterior maxilla displacing roots of maxillary canine andpremolars. B): Intra-operative imageshows well circumscribed lesion causing thinning of cortices, lesion wasremoved in to.

Figure 2
A:) Excised specimen cut section shows solid and cystic areas and a thin capsule. B): Photomicrograph showing encapsulated tumor with solid, cystic and hemorrhagic areas. (HE 40x) C): Photomicrograph showing tumor composed of cells arranged in solid nodules, rosettes or duct like structures and plexiform strands at periphery. (HE 100x) D): Photomicrograph showing tumor composed of variable nodules of spindle, cuboidal and columnar epithelial odontogenic cells. (HE 400x)
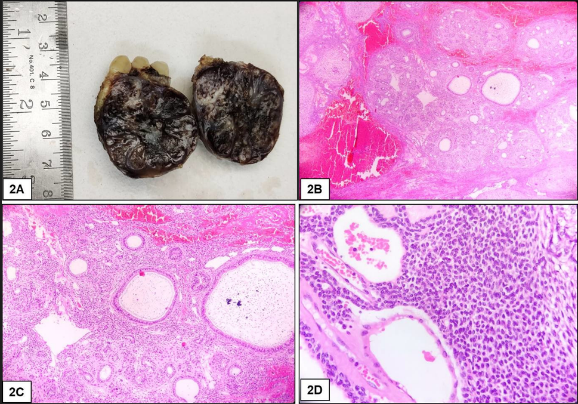
The hematoxylin and eosin stained sections showed encapsulated tumor composed of variable nodules of spindle, cuboidal and columnar epithelial odontogenic cells (Figure 2 B). The cells are arranged in solid nodules, rosettes or duct like structures and plexiform strands at periphery. Few rosettes show eosinophilic secretory material (Figure 2 C). Foci of detinoid matrix, calcification, hemorrhage & hyalinization are identified (Figure 2 D). Separate bits of periosteum are unremarkable. The final diagnosis of Benign epithelial odontogenic tumor - consistent with Adenomatoid Odontogenic tumor was given. The patient was discharged uneventfully.
Discussion
AOT is an uncommonly encountered odontogenic epithelial tumor which has had a debatable past juggling between cyst and tumor, though most evidence and even the present authors opine that AOT is best categorized as an odontogenic tumor. The origin of AOT is controversial, but as it arises in the tooth bearing area, it is thought to arise from the odontogenic epithelium. The nature of AOT ie true neoplasm vs hamartoma has also gained a lot of difference of opinion from various authors. The authors favouring it to be a hamartoma advocated that its limited size, minimal growth potential and the lack of recurrence even after incomplete removal is a feature of hamartomatous lesions. While on the other hand, the small size, anterior location and thus prompt removal prevent excessively large destructive lesion and all these point it to be a true neoplasm.3 The neoplasm has been time and again called as two-thirds tumor pertaining to 2/3rd of the cases affecting the anterior maxilla in females in second to third decade of life. Our patient was also a female in her second decade of life with tumor involving the anterior maxillary region. This odontogenic tumor has three radio graphic variants- Follicular, extrafollicular and peripheral and as a characteristic it is usually small with slow progression.,1, 6 In the present case being discussed, the lesion was a comparatively larger unilocular radiolucency with destruction and resorption of the roots of associated teeth. The histopathological features of adenomatoid odontogenic tumor are characteristic with lesion composed of tumor cells arranged in varying patterns from duct like areas to rosettes, nests, tubules and solid areas. The cells range from spindle to columnar in shape with basal nuclei and clear cytoplasm resembling pre-ameloblasts. Areas of cystic degeneration are commonly present in a fibrous stroma. Calcified deposits and small rounded acellular eosinophilic masses resembling dentinoid admixed with tumour cells are also present.4, 5, 7 The microscopic findings were similar in the present case also along with peripheral areas of the tumor showing plexiform strands of odontogenic epithelium. The common differential diagnosis of AOT can include odontogenic cysts if there is extensive cystic change in the lesion or dentigerous cyst if AOT is associated with a dental follicle. While diagnosing AOT, differentiating it from ameloblastoma is important considering the locally aggressive nature and high growth potential for ameloblastomas.8
Treatment is usually conservative with complete surgical excision/ enucleation of the tumor along with proper follow up. Recurrence has not been reported following proper surgical removal of the tumor. Our patient has been under follow up for last one year without any recurrence.
Conclusion
In conclusion, adenomatoid odontogenic tumor (AOT) is a rare and benign encapsulated neoplasm arising from the odontogenic epithelium. Its classification as a cyst or tumor has been debated, but the latest WHO classification 5th edition, categorizes it as a benign epithelial odontogenic tumor. Histopathologically, it exhibits characteristic rosette or duct-like structures and shows indolent behavior. We presented a case of AOT in a 28-year-old female involving the anterior maxilla with typical histopathological features. Proper surgical excision is the treatment of choice, and recurrence is rare. AOT should be differentiated from other odontogenic cysts and tumors, especially ameloblastoma due to its aggressive nature.

