Introduction
To remove fat, skin slackness, and extra skin with the abdominal skin fold abdominoplasty is contemplated. It is a relatively invasive extraperitoneal technique and generally done with or without liposuction. The ambulatory office-based abdominoplasty procedures are increased because of the lesser price and worldwide availability of plastic surgeons. It also gives an improved and safer anaesthetic procedure.1 Abdominoplasty can be carried out safely under subarachnoid or epidural anaesthesia, even though general anaesthesia is often used for it.2, 3, 4 Subarachnoid anaesthesia is a secure, convenient, expectable, and of lower cost than epidural or general anaesthesia.5 There are many advantages of spinal anaesthesia, the most important being decrease in the incidence of venous thrombotic disease as it permits early ambulation.6, 7, 8
Morbidly obese patients with compromised heart ailment undergoing abdominoplasty pose exceptional challenges to the anaesthesiologist. It is necessary to use the anaesthetic procedure such that it causes minimal haemodynamic instabilities with supreme safety for the patient. The spinal anaesthesia can reduce the rate of occurrence of pulmonary embolism; hence it is of great advantage to the patient. It provides rapid onset, prolonged duration when combined with epidural and can also be used for postoperative analgesia. We report an interesting and challenging case of an abdominoplasty of a 53-year-old, morbidly obese male patient with a body mass index (BMI) of 43.8 Kg/m2 having comorbidities such as chronic kidney disease, obstructive sleep apnea, ventricular bigeminy and severe pulmonary hypertension.
Case Report
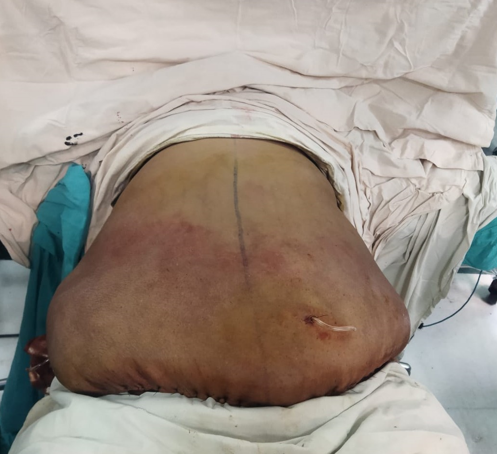
A 53-year-old male, morbidly obese patient with a body mass index (BMI) of 43.8 Kg/m2(Height:185cm, weight:150 Kg) belonging to ASA grade IV, and overhanging abdomen till the level of knee was posted for abdominoplasty (Figure 1). He was diagnosed with chronic kidney disease, obstructive sleep apnea, ventricular bigeminy and severe pulmonary hypertension. Haemogram, serum electrolytes, blood sugar level, coagulation profile, chest X-ray, spirometry and baseline arterial blood gas were normal. Blood urea and serum creatinine levels were 51 mg/dL and 1.59 mg/dL respectively. Venous Doppler ultrasound of lower limbs to rule out deep venous thrombosis was normal. His electrocardiogram was suggestive of ventricular bigeminy and 2D electrocardiography showed dilated right atrium, dilated right ventricle, severe pulmonary hypertension (71 mm of Hg), grade I left ventricular diastolic dysfunction and an ejection fraction of 55.0%.
Table 1
Hemodynamic parameters during the procedure
The patient was nil by mouth for 6 hours before the surgery and was preloaded with one litre of ringer lactate solution overnight. In the operation theatre, the heart rate, non-invasive blood pressure, respiratory rate, oxygen saturation and temperature were monitored. Two large bore intravenous cannulas were secured and intravenous ringer lactate was administered. An 18 G epidural catheter was introduced into T11-T12 intervertebral space using Tuohy needle. Using the loss of resistance to air technique the epidural space was recognized at 6 cm from the skin. The catheter was secured 11 cm on the skin. A subarachnoid block with 2 mL of 0.5% of hyperbaric bupivacaine with 10 µg of fentanylwas administered intrathecally into L3-L4 intervertebral space by using a 25 G Quincke Babcock spinal needle. The dermatomal level was checked 5 min and 10 min after giving spinal anaesthesia by pin prick method. The height of sensory blockade achieved was T10 and T8 respectively. A 10 mL of 0.5% bupivacaine was administered in the epidural catheter 10 minutes after giving the subarachnoid block. The dermatomal level was again evaluated at 3, 5 and 10 minutes after administering epidural dose. T7, T6 and T4 sensory level blockade were achieved accordingly. Motor blockade was assessed using Bromage scale and it was grade 3 at the end of 15 min. The hemodynamic parameters such as heart rate, respiratory rate, non-invasive blood pressure, SpO2 were stable during the procedure (Table 1). The duration of the surgery was 2 hours and 30 minutes. The patient was well hydrated before, during and after the procedure. The sequential compression device was also applied intraoperatively and postoperatively. Postoperative pain relief was provided through epidural catheter. The follow-up of the patient was done till discharge from the hospital (3 days). No complications were observed post-operatively (Figure 2).
Discussion
Morbidly obese patients undergoing abdominoplasty are usually administered general anaesthesia because of patient comfort and better control of airway. There is increased risk of perioperative morbidity and mortality in patients with pulmonary hypertension irrespective of the technique used for anaesthesia.9 Morbid obesity is often associated with CO2 retention and hypoxia due to decreased functional residual capacity. Chronic CO2 retention and hypoxia along with obstructive sleep apnea is often a causative factor or exaggerating factor for pulmonary hypertension. Stress, pain, acidosis, hypoxemia or hypercarbia which are often encountered during the surgery may increase pulmonary hypertension and precipitate right ventricular decompensation.9 Extensive resection in abdominoplasty causing severe pain may require opioids for pain relief which in turn decreases the respiratory drive postoperatively. The combined spinal epidural technique which prevents above precipitating factors is the method of choice in patients with moderate-severe pulmonary hypertension. Low concentration local anaesthetics along with or without low dose opioids provide excellent pain relief in post operative period.
Proper preoperative counselling, preoperative patient optimization and patient co-operation during the procedure are essential. Regional anaesthesia can pose unique challenges like patient positioning, patient discomfort, obscurity of landmarks, loss of control on airway and hemodynamics. It also requires vigilant intraoperative, postoperative monitoring and helps in postoperative pain relief. Abdominoplasty can be performed safely under combined spinal-epidural anaesthesia even though general anaesthesia is regularly used for abdominoplasty.2, 3, 4
Abdominoplasty is associated with a 1.1 % risk of deep venous thrombosis (DVT), which can lead to pulmonary thromboembolism.10 It remains the greatest cause of morbidity and mortality in abdominoplasty surgeries. This has mainly been attributed to increased intraabdominal pressure, which decreases venous return and leads to venous stasis and thus thrombosis. A previous study has implicated general anaesthesia as one of the risk factors for increased intraabdominal pressure.11 But it’s occurrence can be reduced by giving a spinal anaesthesia. Studies in the past also implicate that epidural anaesthesia is known to reduce postoperative thromboembolic complications.2
It was reported that that higher rates of DVT were associated with other plastic surgeries as compared to abdominoplasty procedure.12 It was observed that general anaesthesia was associated with higher rates of DVT as compared to regional anaesthesia. The study further stated that operations lasting more than 3 hours should preferably be performed under regional anaesthesia.13 Local and supervised anesthesia care with or without intravenous sedation is superior to neuraxial blockade, and patient’s safety is better with neuraxial blockade as compared to general anesthesia.14 General anesthesia is associated with more postoperative complications, such as nausea, vomiting, and shivering, than spinal anesthesia, but for extensive dissection general anesthesia was more comfortable for patient and surgeon with long-time procedures particularly exceeding 3 hours.15
Abdominoplasty is sometimes done as an office-based procedure. As the present patient was a high-risk category, it was not conducted as an office-based procedure. The present case report corroborates the possibility of abdominoplasty in a morbidly obese patient under spinal and epidural anaesthesia. Compared with general anaesthesia, a regional anaesthesia for abdominoplasty is considered to have some preferences. Patients may complain of dyspnoea if they have firmly closed abdominoplasties. Patients are conscious and oriented and have fewer postoperative complications.14 The neuraxial blockade should be performed to cover T6 level for successful completion of abdominoplasty under regional anaesthesia.
Metry AA et al. concluded that spinal anaesthesia can be a successful anaesthetic procedure for abdominoplasty when it does not exceed 3 hours duration.15 Burns SM and Meland NB demonstrated that in judiciously selected patients’, abdominoplasty can be performed under spinal anaesthesia as an office-based plastic surgery procedure.16 Neaman KC and Hansen JE in the review of 206 cases regarding the complications of abdominoplasty reported that obese patients had a considerably higher risk of developing major complications as compared with non-obese patients (53.4% versus 28.8%, p-value = 0.001).7