Introduction
Straatsma syndrome, first described by Straatsma in 1979, is a rare condition characterized by amblyopia, nystagmus, and myopia, often associated with abnormal persistence of myelinated nerve fibers in the retina. The prevalence of myelinated nerve fibers is estimated at 0.54% of eyes, with bilateral involvement in a minority of cases and no gender predilection. Diagnosis is primarily clinical, and the condition is typically non-progressive. Myelination of retinal nerve fibers begins around the fifth month of gestation and is completed before birth, facilitated by the lamina cribrosa which normally acts as a barrier. Disruption of this barrier may result in myelination persistence. Blurring of retinal images during critical developmental stages can induce axial elongation and myopia, potentially delaying lamina cribrosa development and allowing for myelination extension. Rare cases of reverse Straatsma syndrome, characterized by unilateral myelinated retinal nerve fibers, amblyopia, and hyperopia, have also been reported.1, 2, 3, 4
Case Report
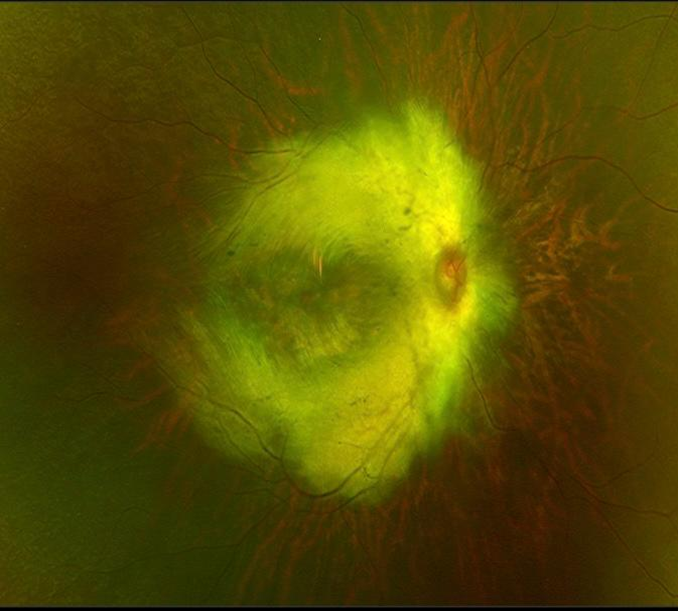
We present an unusual case of a 10-year-old boy with bilateral Straatsma syndrome. He presented with horizontal pendular nystagmus and severely reduced vision since birth, with visual acuity of 2/60 in both eyes corrected to -16 diopters. Fundus examination revealed myopic changes and an anomalous optic disc with extensive myelinated nerve fibers extending across the retina, including the fovea. Axial length measurements were 28.34 mm and 27.96 mm in the right and left eyes, respectively. SD-OCT imaging confirmed significant thickening of the retinal nerve fiber layer. The patient was managed with cycloplegic refraction and occlusion therapy, and regular follow-up examinations every three months were conducted, with the use of contact lenses and cycloplegic refraction.
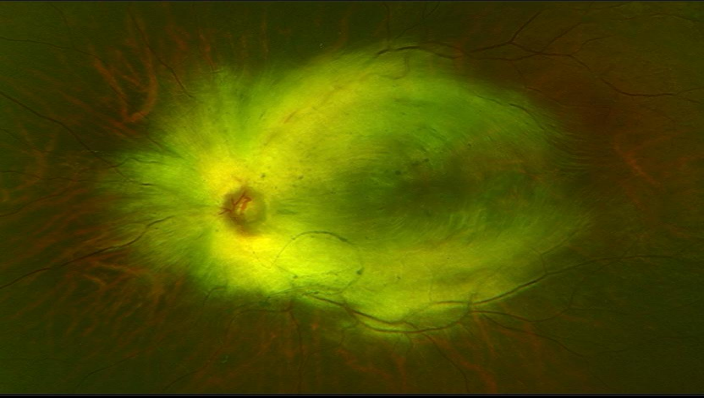
Figure 1
Fundus image showing symmetrical concentricmyelinated nerve fibers involving macula contiguous with optic disc in right eye.
Discussion
Myelinated retinal nerve fibers (MRNF) represent a rare clinical finding affecting approximately 1% of the population. Normally, the myelin sheath is situated behind the lamina cribrosa on retinal nerve fibers. However, in MRNF, the myelin sheath anomalously appears anteriorly as a white striated spot with feathery edges in the peripapillary region. 5 MRNF is typically benign but can variably impact visual function depending on the extent and location of myelinated plaques, including macular involvement. In rare instances, MRNF may be associated with additional ophthalmic conditions such as myopia and amblyopia, collectively termed Straatsma syndrome. Straatsma syndrome can also manifest with nystagmus, strabismus, optic disc hypoplasia, and heterochromia iridium.
Visual prognosis in Straatsma syndrome remains generally poor despite comprehensive treatment including occlusion therapy and full refractive correction, particularly in cases with anisometropia, strabismus, extensive myelination, and macular involvement. Successful treatment of amblyopia can be challenging, with the degree of anisometropia serving as a crucial prognostic determinant; lower levels of anisometropia correlate with better visual outcomes following cycloplegic refraction and intensive occlusion therapy. Strabismus in Straatsma syndrome also contributes to a poorer visual prognosis. 6
MRNF can be categorized into three types based on their location relative to the optic disc: type 1 involves the upper temporal arcade and continues with the optic disc; type 2 is present in both arcades and extends to the optic disc; and type 3 lacks continuity with the optic disc. Among these, type 1 is most prevalent, while type 2 tends to exhibit worse visual outcomes. 7
Previous studies have suggested that an organic etiology, characterized by abnormal foveal appearance on fundus examination and disrupted ellipsoid zone on OCT, predicts a poorer response to occlusion therapy in MRNF patients.
Conclusion
In conclusion, poor prognostic factors in Straatsma syndrome include high levels of anisometropia, presence of strabismus, type 2 MRNF with macular involvement, and delayed initiation of occlusion therapy. Extensive myelination also negatively impacts visual acuity, although limited myelination may similarly be associated with poor visual outcomes. Despite the generally bleak visual prognosis associated with Straatsma syndrome, aggressive occlusion therapy alongside cycloplegic refraction should always be considered.